Our experienced team of doctors at Bay Bariatrics specializes in several surgical procedures to help you achieve your desired weight through metabolic and bariatric surgery. You don’t have to feel alone or out of options if you’ve tried to lose weight and been unsuccessful. We are here to walk beside you on your path to freedom, and our life-changing weight loss surgery will help you live a more active, attractive, and healthy life. Gastric sleeve surgery is one of the bariatric surgery options we offer to help begin your weight loss journey. Give us a call today to schedule your appointment and learn more about Gastric sleeve surgery.
Gastric Sleeve Surgery
Our experienced team of doctors at Bay Bariatrics specializes in several surgical procedures to help you achieve your desired weight through metabolic and bariatric surgery. You don’t have to feel alone or out of options if you’ve tried to lose weight and been unsuccessful. We are here to walk beside you on your path to freedom, and our life-changing weight loss surgery will help you live a more active, attractive, and healthy life. Gastric sleeve surgery is one of the bariatric surgery options we offer to help begin your weight loss journey. Give us a call today to schedule your appointment and learn more about Gastric sleeve surgery.
Life changes dramatically after gastric sleeve surgery.
Improved quality of life
Hunger sensation is decreased
The desire to eat decreases
Easier to develop regular exercise habits
Obesity-related health disorders such as type 2 diabetes, hypertension, sleep apnea, fatty liver disease, joint discomfort, and hyperlipidemia remission or improvement
Weight reduction of 60-70 percent in the first year after surgery
Jennifer Houston-Mayo
“I struggled with weight loss for 20 years. In 2020 I had the gastric sleeve and I have lost 132lbs. I am now able to take better care of myself and my family. I regret not having surgery sooner! Thank you, Bay Bariatrics!”

What is Gastric Sleeve Surgery?
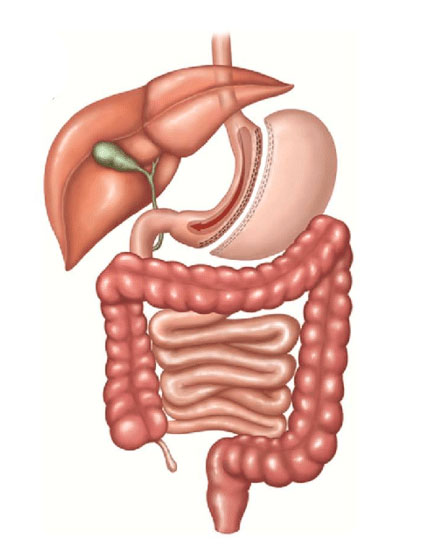
Gastric Sleeve, sometimes known as vertical sleeve gastrectomy, is a surgical technique for weight loss. Laparoscopic sleeve gastrectomy is the most commonly performed bariatric surgery in the United States and worldwide. This operation is usually done laparoscopically, which includes putting small instruments into the upper part of the stomach through several small incisions. Roughly 80% of the stomach is removed during a sleeve gastrectomy, leaving a tube-shaped stomach about the size and shape of a banana.
The amount of food you can ingest is limited by the size of your stomach. Furthermore, the operation causes hormonal changes that aid weight loss. The same hormonal changes that help people lose weight also help improve conditions associated with obesity, like high blood pressure and heart disease.
More FAQs About Gastric Sleeve
What qualifies a person for gastric sleeve?
Our experienced team of surgeons at Bay Bariatrics has several criteria to help determine what bariatric procedures may be right for you. Our goal is to help you qualify for the weight loss surgery that will be the most successful for your unique needs. Whether it is gastric sleeve or gastric bypass surgery, if you have a body mass index (BMI) of 35-40 with certain serious health concerns like Type 2 diabetes, sleep apnea, or high blood pressure, you may be a candidate for bariatric surgery. It is also possible to qualify with a BMI greater than 40, and some ethnic groups qualify with lower BMI numbers. Call our office today to schedule an appointment and learn more about losing weight through gastric sleeve surgery.
How much weight can you lose with a gastric sleeve?
For approximately 6-12 months after bariatric surgery, most patients lose 2-4 pounds (0.9-1.8kg) per week. This results in an average monthly weight loss of 8 to 16 pounds for most patients. Typically, you should expect to lose up to 70% of your excess weight. From your baseline starting point, the sleeve gastrectomy often leads to 25 to 35 percent body weight loss or 50 to 70 percent excess weight loss. The difference between your ideal and current weight is your excess body weight. Significant weight loss is just one advantage of gastric sleeve.
What are the advantages of the gastric sleeve versus the gastric bypass surgery?
The fundamental benefit of gastric sleeve surgery is that no new connection between the stomach and small bowel is required (anastomosis). With gastric sleeve surgery, long-term problems are less likely than with gastric bypass surgery. Because there is no anastomosis, there is essentially little risk of internal hernia or marginal ulcers after gastric sleeve surgery. Gastric bypass patients report these problems most commonly. Because there is no malabsorption, nutrient deficiency is less likely with gastric sleeve surgery than with gastric bypass surgery. Vitamin and mineral supplements are recommended with both laparoscopic surgery procedures. Our surgeons at Bay Bariatrics can help you understand the benefits of both sleeve gastrectomy and gastric bypass surgery and help determine which weight loss surgery is best for you.
Will the gastric sleeve cause heartburn?
Following gastric sleeve surgery, certain clinics observed an increase in cases of Gastroesophageal Reflux Disease (GERD). Other reports, however, revealed a reduction in GERD cases. Acid reflux (heartburn) caused by gastric sleeve surgery may typically be controlled with antacid medicines and lifestyle changes. To address reflux, doctors will rarely have to convert the gastric sleeve to the Roux-en-Y gastric bypass procedure (less than 1 percent).
According to studies, one of the reasons individuals have reflux following gastric sleeve surgery is a retained fundus (the top section of the stomach). Our skilled surgeons at Bay Bariatrics pay close attention to this part of the procedure to ensure that the whole stomach fundus is removed during gastric sleeve surgery. Our goal is to minimize any potential side effects and maximize your potential to shed excess weight.
Can my stomach grow back after gastric sleeve?
Overeating can contribute to weight gain. When someone overeats, their stomach expands to accommodate the extra food. Patients who are having gastric sleeve surgery should be aware of this. Your stomach will expand every time you consume something. However, if you eat past the point of fullness on a regular basis, you risk extending your stomach beyond the size that it was right after surgery.
The brain can get confused about when it’s time to eat or when it’s full if the stomach becomes stretched. When your stomach is stretched beyond its typical size, your brain feels you need more food to be satisfied. Alternatively, after eating until satisfied and digesting a portion of the meal, your brain may assume that the body requires additional food because the stomach is no longer empty.
When you consume large meals over and over again, your stomach stretches. This may not be a problem if you overeat on occasion during holidays or celebrations. However, if this happens frequently, stomach stretching is more likely. For instance, if you eat a huge breakfast, lunch, and dinner every day for a few weeks, your stomach will stretch. The altering of the fullness gauge causes you to overeat beyond your body’s level of fullness and is what causes you to regain weight, not the actual stretching of the stomach.
How long does a gastric sleeve last?
Studies show that sleeve gastrectomy is still successful almost six years later, with about 60% of extra BMI gone and comorbidities showing substantial improvement or even remission. Our surgeons at Bay Bariatrics specialize in bariatric surgery procedures that offer long-term solutions for your weight loss needs.
What is a typical diet after gastric sleeve?
You will be on a liquid diet for the first few days after your gastric sleeve procedure. Shortly thereafter, you will transition to pureed foods, then to soft foods, and finally to solid foods. Developing good eating habits such as avoiding eating too much food will help your body recover and adjust to your new smaller stomach.
Your doctor will thoroughly go over your dietary guidelines including the amount of food you should eat and answer any questions about your new healthy diet. Significant weight loss can only be achieved by adhering to the dietary guidelines strictly. You can expect to restrict both calories and carbohydrates like sweets, potatoes, and pasta. Lean protein, vegetables, and low-or no-calorie water will be your staples. Your doctor may even prescribe a daily calorie goal for you to follow.
Can you drink alcohol after gastric sleeve?
For the first six months after bariatric surgery, you should avoid alcohol. It is best to stay away from carbonated beverages and sugary drink mixers once you’ve received clearance to resume drinking alcohol. Even small amounts of alcohol can cause intoxication and low blood sugar levels following surgery.
To help slow the absorption of alcohol, only drink with meals or while eating. You should also keep in mind that alcohol has a high-calorie content and can cause you to gain weight when not consumed in moderation. If you find yourself drinking to cope with emotions or stress on a frequent basis, seek help from your doctor.
What foods cannot be eaten after gastric sleeve surgery?
Gastric sleeve patients need to make smart dietary decisions to ensure their body gets adequate nutrients every day. Avoiding items with little or no nutritional value is part of a bariatric surgery diet. Pastries, sweets, chips, pretzels, rice cakes, and popcorn are all examples of foods you should avoid. If you eat these items, you risk becoming malnourished or regaining weight. Sugary or fried foods might cause a condition known as “dumping syndrome,” in which these foods are promptly emptied into the colon after consumption. Dumping syndrome is characterized by weakness, cold sweats, nausea, vomiting, and diarrhea.
How many liquids should you consume after gastric sleeve?
Doctors recommend that patients drink two liters (or eight glasses) of water (or caffeine-free drinks) every day after sleeve gastrectomy surgery. It’s crucial to remember not to drink beverages with food for at least 30 minutes before or after eating. This is an important part of any bariatric surgery diet since it will make you feel full and free up space in your pouch for nutrients.
What Is Duodenal Switch Surgery?
Duodenal switch surgery begins with a vertical sleeve gastrectomy, which is purposefully made slightly bigger than when a gastric sleeve surgery is conducted as a stand-alone treatment. This is done to allow for more protein-rich meals to be consumed.
The pylorus, a valve within the digestive tract, marks the boundary between the stomach and the first segment of the intestine, or the duodenum. The duodenum is separated around one inch beyond this boundary. An intestinal bypass is used to restore a connection to food. This has traditionally been done in the same way as a Roux-en-Y Gastric Bypass. A duodenal switch, on the other hand, bypasses more bowel. As a result, the procedure is classified as malabsorptive, which means that part of the nutrients ingested by the gut are not absorbed. As a result, more vitamin and mineral supplements are required for adequate nutrition.
The procedure decreases the blood sugar fluctuations that are common with gastric bypass. Nutritional deficits and diarrhea are thought to be reduced when less bowel is bypassed.

Cheer P. - Lost 130 lbs.
I was 30 years old and felt like an invisible person at 280 lbs. I didn’t think anyone would hire me. After my surgery, I lost 130 lbs and have kept that weight off for more than a decade. Since my surgery, I’m more confident, completed school and had a third child. I love being able to keep up my kids and their activities.
